Researchers at two Ontario universities have developed a pain-free, wearable sensor that can continuously monitor levels of blood sugar, lactates and other critical health indicators for weeks at a time, sending results to a smartphone or other device.
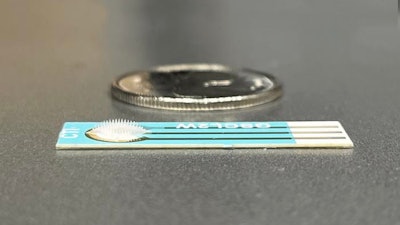
The Wearable Aptalyzer, created by a team featuring researchers from McMaster University and the University of Waterloo, uses an array of tiny hydrogel needles that penetrate just deeply enough to reach the interstitial fluid beneath the skin, but not far enough to reach the blood vessels or nerves.
The patch gathers and sends information about markers in the fluid to an electronic device such as a smart phone, creating an ongoing record of patterns in the rise and fall of critical biomarkers.
Once developed for clinical use, it will allow health professionals to access current medical information that today is available only retrospectively after blood tests and lab work.
The new technology could make monitoring the markers of specific diseases and conditions as simple as tracking pulse, blood pressure and other vital signs. The researchers describe the work in a new paper published today in the journal Advanced Materials.
“This technology can provide real-time information about both chronic and acute health conditions, allowing caregivers to act more quickly and with greater certainty when they see trouble,” says one of the paper’s two corresponding authors, McMaster’s Leyla Soleymani, professor of Engineering Physics who holds the Canada Research Chair in Miniaturized Biomedical Devices.
“The Wearable Aptalyzer is a general platform, meaning it can measure any biomarkers of interest, ranging from diabetes to cardiac biomarkers,” says corresponding author Mahla Poudineh, an assistant professor and director of the IDEATION Lab in the Department of Electrical and Computer Engineering at Waterloo. “Continuous health monitoring doesn't just help catch diseases early and track how treatments are working. It also helps us understand how diseases happen, filling in important gaps in our knowledge that need attention.”
A user would apply and remove the patch much like a small bandage held in place with barely visible, soft hooks. The convenience is likely to appeal to diabetics and others who test themselves by drawing samples of blood or by using solid monitoring patches with metal needles that penetrate deeper and rely on less specific electrodes.
The greatest promise of the technology, though, may lie in its ability to produce weeks’ worth of meaningful results at a time, and to transmit data to electronic devices experts can read without sophisticated equipment.
Among the other potential applications, the Wearable Aptalyzer can make it possible to read and send data that signals cardiac events in real time, making it a potentially valuable tool for monitoring patients in ambulances and emergency rooms, and during treatment. The same technology can readily be adapted to monitor the progress and treatment of many chronic illnesses, including cancers, the researchers say.
The technology holds promise for improving care use in remote care settings, such as northern Indigenous communities set far from hospitals, or on space flights. Data from the Wearable Aptalyzer can signal trouble before symptoms become apparent, making it more likely patients can receive timely care.
The next steps in developing the technology for broad use include human trials and regulatory approvals. The researchers are seeking partners to help commercialize the technology.
The paper’s lead authors are Fatemeh Bakhshandeh of McMaster and Hanjia Zheng of Waterloo. Together with Soleymani and Poudineh, their co-authors are Waterloo’s Sadegh Sadeghzadeh, Irfani Ausri, Fatemeh Keyvani, Fasih Rahman, Joe Quadrilatero, and Juewen Liu, and McMaster’s Nicole Barra, Payel Sen, and Jonathan Schertzer.






















