By injecting a solution of nanoparticles around the heart, a temporary heart stimulator self-assembles, which can correct heart arrhythmia in emergency situations with the help of an external power source. After treatment, the electrode spontaneously disappears from the body. The study was conducted on animals.
Arrhythmia occurs when there are disturbances in the heart’s electrical signals, causing it to beat too fast, slow, or irregularly. Often, arrhythmia can be treated with medication, but it is also possible to alter the heart's rhythm using electrical signals with, for example, a defibrillator or surgically implanted pacemaker. These types of interventions can be challenging in war zones, during mountain hikes, or in other environments where a defibrillator is not available or surgery is not feasible.
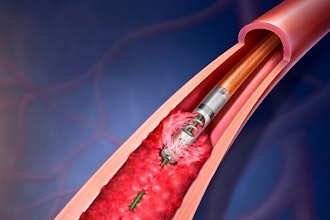
"We have developed an injectable heart stimulator for emergency situations, which consists of a syringe loaded with a solution of nanoparticles," says Roger Olsson, Professor of Chemical Biology and Therapeutics at Lund University and Professor of Medicinal Chemistry at the University of Gothenburg.
Nanoparticles are extremely small particles. Because the particles are so small, they can be injected with a needle thinner than a human hair. When the solution comes into contact with tissue, a structure forms around the heart consisting of a long chain of molecules—a so-called polymer—that conducts electricity. The injected electrode integrates with the body’s cells and facilitates ECG measurements, can regulate heartbeats, and correct arrhythmia.
"If you connect a mobile phone to the injection site near the heart, you can temporarily stimulate the heart's rhythm for up to five days," says Umut Aydemir, a doctoral student and first author of the study.
Owing to the intimate contact between the polymer and the heart tissue, the stimulator can operate with low power inputs which can come from handheld devices. Most people carry their mobile phones everywhere, and with the help of a cable attached to the skin at the injection site near the heart, charges from the phone can be transferred to the conductive electrode in the body. With an app on the phone—which the researchers now want to develop—you can then regulate the arrhythmia before the person in question can reach a hospital for further treatment.
So far, these experimental studies have been on small animals, zebrafish and chicken embryos, following the 3R principle to reduce animal testing in mammals. Now that the concept is optimized and shows great potential, the next step is studies in larger animals, such as pigs, for translation to humans.
"The method is minimally invasive. Moreover, the heart stimulator spontaneously degrades and is excreted from the body after treatment, so it does not need to be surgically removed," concludes Martin Hjort, Associate Researcher in Chemical Biology and Therapeutics at Lund University.